Hypertension in pregnancy and its related complications, such as Preeclampsia, can have significant implications in the health and safety of birthing individuals and their babies. Prior to 2007, these conditions were more rare in otherwise healthy pregnancies. Studies have shown, though, that Chronic Hypertension in Pregnancy doubled between 2007-2021 (source).
Understanding what these conditions are, how they are diagnosed, and what symptoms to watch for is key to early detection and effective treatment. With early intervention and treatment, pregnancy outcomes have a high probability to be positive even after diagnosis. In this post, we will explore hypertension in pregnancy and preeclampsia including symptoms, how these conditions are diagnosed, and variations or other related diagnoses.
Hypertension in Pregnancy
What is Chronic Hypertension in Pregnancy?
Chronic hypertension in pregnancy is defined as high blood pressure that either exists prior to pregnancy, is diagnosed within the first 20 weeks of pregnancy, or does not resolve by the 12-week postpartum checkup. According to this article, Chronic Hypertension affects at estimated 5% of pregnancies.
What is Gestational Hypertension in Pregnancy?
The main difference between Chronic Hypertension and Gestational Hypertension in pregnancy is that Gestational Hypertension (formerly known as Pregnancy-Induced Hypertension or PIH) is new Hypertension that is diagnosed after 20 weeks of pregnancy. This condition is unique in that it is diagnosed after birth if you don’t develop preeclampsia and your blood pressure returns to normal after 12 weeks postpartum.
While this makes it sound less severe than Preeclampsia, it’s of note that if this condition progresses from mild to severe Gestational Hypertension the treatment is very similar to severe Preeclampsia. Both conditions are important to monitor and intervene if necessary.
Unlike Preeclampsia, Chronic and Gestational Hypertension may not always present with symptoms. However, regular monitoring of blood pressure is essential to ensure early detection.
What Symptoms Should You Watch for?
Pregnant individuals who experience high blood pressure readings (140/90 mmHg or higher), headaches, visual disturbances, or swelling of the face, hands, or feet should discuss with their healthcare provider if further testing is needed.
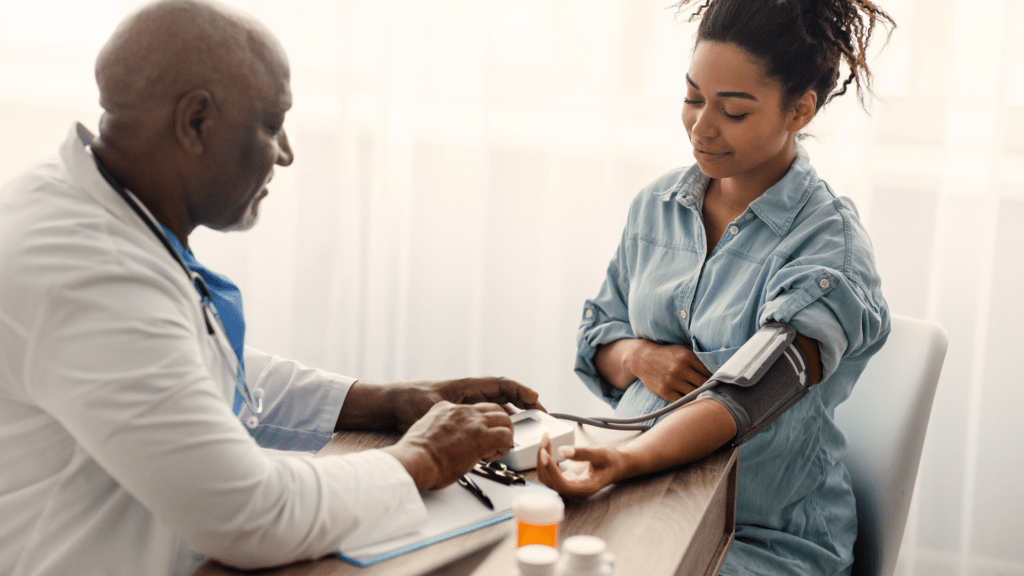
How are Chronic and Gestational Hypertension Diagnosed?
Both Chronic and Gestational Hypertension are diagnosed via blood pressure measurement, urine analysis, and blood tests. Blood pressure tests are always the first line of defense as they’re taken at each routine visit. Urine analysis is also routine however they’ll do a more intensive analysis to rule out Preeclampsia. Blood tests may also be taken to check on organ function.
How Common is Hypertension in Pregnancy?
Hypertension occurs in about 10% of pregnancies in the United States. Chronic Hypertension affects about 1-5% of pregnancies, while Gestational Hypertension affects approximately 6-8%.

Preeclampsia
What is Preeclampsia?
Preeclampsia is a serious condition that typically develops after the 20th week of pregnancy. It is characterized by high blood pressure and damage to organs, most commonly the liver and kidneys. This condition can progress rapidly and pose significant risks to both the pregnant person and the baby. It can potentially lead to complications like preterm birth or placental abruption and can even be fatal if left untreated.
What Symptoms Should You Watch for?
The symptoms of Preeclampsia can range from mild to severe. It’s important that individuals share their symptoms with their healthcare provider no matter the level of intensity. It is possible, however, to have Preeclampsia without these symptoms which is why routine prenatal appointments are important! Just like with Hypertension in Pregnancy, persistent high blood pressure (140/90 mmHg or higher), headaches, visual disturbances, and swelling of face, feet, or hands are common.
Other things to watch for include:
- Excess protein in the urine (proteinuria)
- Upper abdominal pain, particularly under the ribs on the right side
- Nausea or vomiting
- Sudden weight gain
- Shortness of breath
How is Preeclampsia Diagnosed?
If Preeclampsia is suspected, the first step will typically be to get a reading on blood pressure followed by a urine analysis. When readings are consistently at 140/90 mmHg or higher and there is protein present in the urine, healthcare providers will typically move forward with a blood test to check on liver and kidney function and platelet counts as well as an ultrasound and non-stress test (NST) to monitor the baby’s growth as restricted fetal development can be common in Preeclampsia.
How Common is Preeclampsia?
Preeclampsia affects about 5-8% of pregnancies in the U.S. It is most common in first-time pregnancies, but risk factors include being pregnant with multiples (twins or more) and a history of hypertension or kidney disease.
How Common is Postpartum Preeclampsia?
Postpartum Preeclampsia is rare, occurring in about 0.3-0.7% of pregnancies. It can occur in individuals who had Preeclampsia during pregnancy, but it may also develop in individuals with no prior related history. The symptoms remain the same during pregnancy and after delivery. Postpartum Preeclampsia can develop after a baby has been delivered. The highest risk is 48 hours after delivery but it’s important to pay attention to symptoms that develop once you’ve arrived home and seek care immediately if something appears to be off.
Are There Other Conditions I Need to be Aware of?
The other main hypertension-related condition to be aware of is HELLP (Hemolysis, Elevated Liver enzymes and Low Platelets) syndrome. HELLP previously was thought to be its own classification. It is now thought to fall under the hypertension umbrella as a variation of Preeclampsia. This condition can be more difficult to diagnose because the early symptoms present just like Preeclampsia symptoms. This is why it’s important to know the symptoms, attend your routine prenatal appointments, and intervene early. Preeclampsia.org estimates that of the 5-8% of pregnancies that develop Preeclampsia, 15% of these people develop HELLP (source).
Hypertension and its related conditions are significant health concerns for pregnant and postpartum individuals. These conditions, while statistically more rare, are still important to pay attention to and know the symptoms of.
During pregnancy it is important to attend routine appointments for a whole host of reasons! Early detection of conditions like Hypertension is just one. Remember, even if a pregnant individual develops one of the conditions we’ve noted here, treatment is possible! Outcomes are greatly impacted by early intervention.
Struggling with one or more of the symptoms above? We want to encourage you to reach out to your doula and healthcare provider immediately. Chances are you’re okay (statistically speaking!) but the peace of mind from double checking is invaluable.